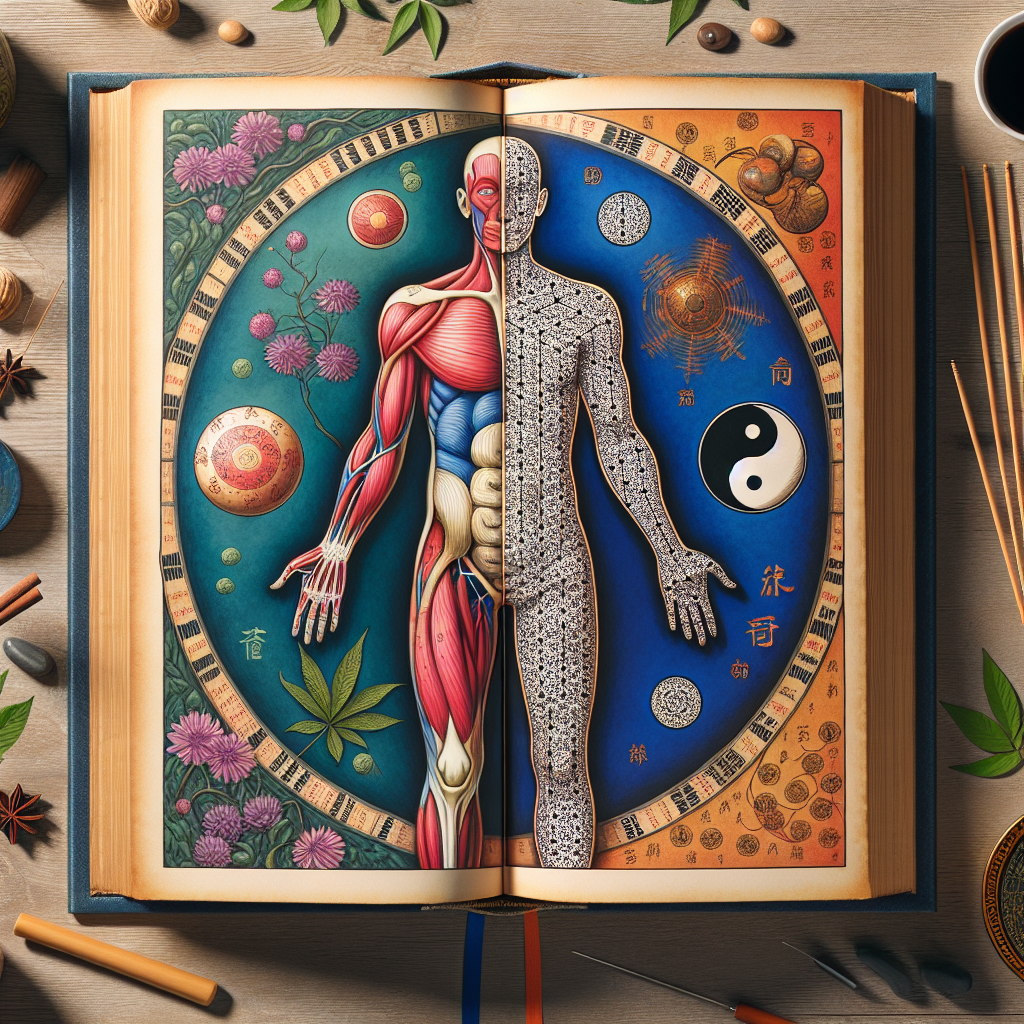
Integrating Healing Traditions: A Comprehensive Guide to Treating Chronic Fatigue Syndrome with Western Medicine and Eastern Therapies
Chronic Fatigue Syndrome (CFS), also known as Myalgic Encephalomyelitis (ME), is a complex, long-term illness characterized by extreme fatigue that is not improved by rest and is worsened by physical or mental activity. It is a condition that mystifies many, partly because its causes remain incompletely understood and its symptoms overlap with various other conditions. Patients often find themselves navigating a labyrinth of treatments, encountering both Western medical approaches and Eastern healing traditions along their journey.
Understanding Chronic Fatigue Syndrome
The diagnosis of CFS is challenging. It requires a thorough examination to exclude other potential causes of fatigue, such as thyroid issues, depression, and autoimmune diseases. Symptoms include profound tiredness, sleep abnormalities, cognitive difficulties, and sometimes muscle and joint pain. The intense fatigue experienced by CFS sufferers significantly impairs their daily functioning, making effective treatment strategies a necessity.
Western Medicine Approach
In the Western medical paradigm, treatment for CFS is largely symptomatic, focusing on managing symptoms and improving quality of life. There is no known cure, and treatments are tailored to the individual’s symptoms. Approaches may include:
– Pharmacological Treatments: These can include pain relievers, sleep aids, and sometimes low-dose antidepressants to aid sleep and address pain. Stimulants may be considered for severe cases but are used cautiously due to the potential for worsening symptoms.
– Cognitive Behavioral Therapy (CBT): CBT is used to help manage the illness by changing how patients perceive their condition, improving coping strategies, and gradually increasing activity levels within tolerance.
– Graded Exercise Therapy (GET): Initially controversial, GET involves careful, gradual increases in physical activity to improve energy levels and function. The effectiveness and appropriateness of GET have been debated, with recent guidelines emphasizing patient-centered approaches and pacing.
Eastern Healing Traditions
Eastern therapies offer a holistic view, focusing on restoring balance within the body’s energy systems and enhancing overall well-being. While lacking in rigorous clinical trials that Western medicine demands, many patients have reported improvements in symptoms through these modalities, including:
– Acupuncture: Based on traditional Chinese medicine, acupuncture involves inserting thin needles into specific points on the body. It aims to restore energy flow and has been reported to help alleviate pain and improve sleep in CFS patients.
– Yoga and Tai Chi: These practices combine gentle physical movements, breath control, and meditation to enhance physical and mental health. They can help improve flexibility, reduce stress, and increase stamina in a controlled, gradual manner.
– Herbal Medicine: Various herbal remedies, guided by traditional Chinese medicine or other herbal traditions, aim to address underlying imbalances. Herbs like Ginseng and Ashwagandha have been cited for their potential to boost energy and resilience.
Integrating Western and Eastern Approaches
The complexity of CFS, coupled with its multifaceted symptoms, suggests that an integrated approach to treatment might offer the best outcomes for patients. Integrating Western and Eastern therapies involves a delicate balance, ensuring that treatments from both worlds complement rather than contradict each other.
1. Collaborative Care: A team approach that includes doctors, physical therapists, mental health professionals, and practitioners of Eastern medicine can provide a comprehensive treatment plan. Communication among practitioners ensures that therapies are complementary and tailored to individual needs.
2. Evidence-Based Eastern Practices: Patients and practitioners should seek out Eastern therapies with some evidence base or those that have been subject to clinical trials. Practices such as acupuncture and certain forms of meditation have received scientific attention and can be integrated with a degree of confidence.
3. Personalized Treatment Plans: Given the individual nature of CFS, treatment plans should be highly personalized. Some patients may benefit from a greater emphasis on Western pharmacological treatments and CBT, while others find significant relief from acupuncture and herbal medicine. Listening to the patient’s body and adjusting the treatment plan accordingly is crucial.
4. Monitoring and Adjusting: Regular monitoring of symptoms and side effects, with adjustments to the treatment plan as necessary, is key to finding the right balance between Western and Eastern approaches. This iterative process respects the body’s response to various treatments and acknowledges the evolving nature of CFS.
Conclusion
Chronic Fatigue Syndrome remains one of the more challenging conditions to manage, given its unclear etiology, diverse symptomatology, and the absence of a definitive cure. An integrated approach that combines the strengths of Western medicine with the holistic perspectives of Eastern healing traditions offers a promising pathway to managing the condition. By focusing on symptom management, improving quality of life, and addressing underlying imbalances, patients can find a regimen that brings relief and fosters long-term well-being. As research continues to evolve in both realms, the hope is that the integration of these diverse healing traditions will lead to more effective and personalized strategies for managing CFS.